Microcephaly
| Microcephaly | |
|---|---|
 | |
| A baby with microcephaly (left) compared to a baby with a typical head size | |
| Pronunciation | |
| Specialty | Medical genetics, Psychiatry, Neurology |
| Symptoms | Abnormally small head and brain, neurological impairments |
| Complications | Neurological impairments |
| Usual onset | Congenital |
| Duration | Lifelong |
| Causes | Usually genetic or toxin exposure during pregnancy |
| Prevention | Avoiding alcohol consumption while pregnant |
| Frequency | 2–12 per 10,000 births[1] |

Microcephaly (from Neo-Latin microcephalia, from Ancient Greek μικρός mikrós "small" and κεφαλή kephalé "head"[2]) is a medical condition involving a smaller-than-normal head.[3] Microcephaly may be present at birth or it may develop in the first few years of life.[3] Brain development is often affected; people with this disorder often have an intellectual disability, poor motor function, poor speech, abnormal facial features, seizures and dwarfism.[3]
The disorder is caused by a disruption to the genetic processes that form the brain early in pregnancy,[3] though the cause is not identified in most cases.[4] Many genetic syndromes can result in microcephaly, including chromosomal and single-gene conditions, though almost always in combination with other symptoms. Mutations that result solely in microcephaly (primary microcephaly) exist but are less common.[5] External toxins to the embryo, such as alcohol during pregnancy or vertically transmitted infections, can also result in microcephaly.[3] Microcephaly serves as an important neurological indication or warning sign, but no uniformity exists in its definition. It is usually defined as a head circumference (HC) more than two standard deviations below the mean for age and sex.[6][7] Some academics advocate defining it as head circumference more than three standard deviations below the mean for the age and sex.[8]
There is no specific treatment that returns the head size to normal.[3] In general, life expectancy for individuals with microcephaly is reduced, and the prognosis for normal brain function is poor. Occasional cases develop normal intelligence and grow normally (apart from persistently small head circumference).[3][9] It is reported that in the United States, microcephaly occurs in 1 in 800-5,000 births.[4]
Signs and symptoms
[edit]
There are a variety of symptoms that can occur in children. Infants with microcephaly are born with either a normal or reduced head size.[10] Subsequently, the head fails to grow, while the face continues to develop at a normal rate, producing a child with a small head and a receding forehead, and a loose, often wrinkled scalp.[11] As the child grows older, the smallness of the skull becomes more obvious, although the entire body also is often underweight and dwarfed.[10]
Severely impaired intellectual development is common, but disturbances in motor functions may not appear until later in life.[10] Affected newborns generally have striking neurological defects and seizures.[10] Development of motor functions and speech may be delayed. Hyperactivity and intellectual disability are common occurrences, although the degree of each varies. Convulsions may also occur. Motor ability varies, ranging from clumsiness in some to spastic quadriplegia in others.[12]
Causes
[edit]Microcephaly is a type of cephalic disorder. It has been classified in two types based on the onset:[13]
Congenital
[edit]This section needs additional citations for verification. (February 2016) |
- Isolated
- Familial (autosomal recessive) microcephaly[14]
- Autosomal dominant microcephaly[15][16]
- X-linked microcephaly[14]
- Chromosomal (balanced rearrangements and ring chromosome)
- Syndromes
- Chromosomal
- Poland syndrome[17]
- Down syndrome[18]
- Edward syndrome[19]
- Patau syndrome[20]
- Unbalanced rearrangements
- Contiguous gene deletion
- 4p deletion (Wolf–Hirschhorn syndrome)
- 5p deletion (Cri-du-chat)
- 7q11.23 deletion (Williams syndrome)
- 22q11 deletion (DiGeorge syndrome)
- Chromosomal
- Single gene defects
- Acquired
- Disruptive injuries
- Ischemic stroke[23]
- Hemorrhagic stroke[23]
- Death of a monozygotic twin
- Vertically transmitted infections
- Drugs
- Disruptive injuries
- Other
- Radiation exposure to mother
- Maternal malnutrition[24]
- Maternal phenylketonuria[24]
- Poorly controlled gestational diabetes
- Hyperthermia
- Maternal hypothyroidism
- Placental insufficiency
- Craniosynostosis[24]
Postnatal onset
[edit]This section needs additional citations for verification. (February 2016) |
- Genetic
- Syndromes
- Contiguous gene deletion
- 17p13.3 deletion (Miller–Dieker syndrome)[32]
- Single gene defects
- Rett syndrome (primarily girls)
- Nijmegen breakage syndrome
- X-linked lissencephaly with abnormal genitalia
- Aicardi–Goutières syndrome
- Ataxia telangiectasia
- Cohen syndrome
- Cockayne syndrome
- Contiguous gene deletion
- Acquired
- Disruptive injuries
- Infections
- Congenital HIV encephalopathy[34]
- Meningitis[35]
- Encephalitis[36]
- Toxins
- Deprivation
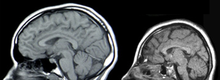
Genetic mutations cause most cases of microcephaly.[3] Relationships have been found between autism, duplications of genes and macrocephaly on one side. On the other side, a relationship has been found between schizophrenia, deletions of genes and microcephaly.[42][43][44] Several genes have been designated "MCPH" genes, after microcephalin (MCPH1), based on their role in brain size and primary microcephaly syndromes when mutated. In addition to microcephalin, these include WDR62 (MCPH2), CDK5RAP2 (MCPH3), KNL1 (MCPH4), ASPM (MCPH5), CENPJ (MCPH6), STIL (MCPH7), CEP135 (MCPH8), CEP152 (MCPH9), ZNF335 (MCPH10), PHC1 (MCPH11) and CDK6 (MCPH12).[5] Moreover, an association has been established between common genetic variants within known microcephaly genes (such as MCPH1 and CDK5RAP2) and normal variation in brain structure as measured with magnetic resonance imaging (MRI)—i.e., primarily brain cortical surface area and total brain volume.[45]
Arbovirus
[edit]Bites and stings from Arthropods can often be a cause of vector-borne diseases. These include mosquitoes, fleas, sand flies, lice, ticks, and mites that are hematophagous vectors. The Centers for Disease Control (CDC) stated that "mosquitoes kill more people than any other creature and considers that mosquitoes are "the most dangerous animals on earth".[46]
The spread of Aedes mosquito-borne Zika virus has been implicated in increasing levels of congenital microcephaly by the International Society for Infectious Diseases and the US Centers for Disease Control and Prevention.[47] Zika can spread from a pregnant woman to her fetus. This can result in other severe brain malformations and birth defects.[48][49][50][51] A study published in The New England Journal of Medicine has documented a case in which they found evidence of the Zika virus in the brain of a fetus that displayed the morphology of microcephaly.[52]
Microlissencephaly
[edit]Microlissencephaly is microcephaly combined with lissencephaly (smooth brain surface due to absent sulci and gyri). Most cases of microlissencephaly are described in consanguineous families, suggesting an autosomal recessive inheritance.[53][54][55]
Historical causes of microcephaly
[edit]After the dropping of atomic bombs "Little Boy" on Hiroshima and "Fat Man" on Nagasaki, several women close to ground zero who had been pregnant at the time gave birth to children with microcephaly.[56] Microcephaly was present in 7 children from a group of 11 pregnant women at 11–17 weeks of gestation who survived the blast at less than 1.2 km (0.75 mi) from ground zero.[57] Due to their proximity to the bomb, the pregnant women's in utero children received a biologically significant radiation dose that was relatively high due to the massive neutron output of the lower explosive-yielding Little Boy.[57] Researchers studied 286 additional children who were in utero during the atomic bombings, and after a year they found these children had a higher incidence of microcephaly and mental retardation.[58][57]
Other relations
[edit]Intracranial volume also affects this pathology, as it is related with the size of the brain.[59]
Pathophysiology
[edit]Microcephaly generally is due to the diminished size of the largest part of the human brain, the cerebral cortex, and the condition can arise during embryonic and fetal development due to insufficient neural stem cell proliferation, impaired or premature neurogenesis, the death of neural stem cells or neurons, or a combination of these factors.[60] Research in animal models such as rodents has found many genes that are required for normal brain growth. For example, the Notch pathway genes regulate the balance between stem cell proliferation and neurogenesis in the stem cell layer known as the ventricular zone, and experimental mutations of many genes can cause microcephaly in mice,[61] similar to human microcephaly.[62][63] Mutations of the abnormal spindle-like microcephaly-associated (ASPM) gene are associated with microcephaly in humans and a knockout model has been developed in ferrets that exhibits severe microcephaly.[64] In addition, viruses such as cytomegalovirus (CMV) or Zika have been shown to infect and kill the primary stem cell of the brain—the radial glial cell, resulting in the loss of future daughter neurons.[65][66] The severity of the condition may depend on the timing of infection during pregnancy.[citation needed]
Microcephaly is a feature common to several different genetic disorders arising from a deficiency in the cellular DNA damage response.[67] Individuals with the following DNA damage response disorders exhibit microcephaly: Nijmegen breakage syndrome, ATR-Seckel syndrome, MCPH1-dependent primary microcephaly disorder, xeroderma pigmentosum complementation group A deficiency, Fanconi anemia, ligase 4 deficiency syndrome and Bloom syndrome. These findings suggest that a normal DNA damage response is critical during brain development, perhaps to protect against induction of apoptosis by DNA damage occurring in neurons.[68]
Treatment
[edit]
There is no known cure for microcephaly.[3] Treatment is symptomatic and supportive.[3] Because some cases of microcephaly and its associated symptoms may be a result of amino acid deficiencies, treatment with amino acids in these cases has been shown to improve symptoms such as seizures and motor function delays.[69]
History
[edit]People with small heads were displayed as a public spectacle in ancient Rome.[70]
People with microcephaly were sometimes sold to freak shows in North America and Europe in the 19th and early 20th centuries, where they were known by the name "pinheads". Many of them were presented as different species (e.g., "monkey man") and described as being the missing link.[71] Famous examples include Zip the Pinhead (although he may not have had microcephaly), Maximo and Bartola and Schlitzie the Pinhead.[72] Stars of the 1932 film Freaks, were cited as influences on the development of the long-running comic strip character Zippy the Pinhead, created by Bill Griffith.[73]
-
18-year-old Emil R., 1868
-
Elderly female, 1888/89
-
52-year-old female, 1900
-
10-year-old male, 1904
-
20-year-old female, 1906/07
-
3 relatives, 1913
-
18-year-old sister and 9-year-old brother, 1917
-
55-year-old female, 1920 (linear descendant of Pocahontas)
-
6 siblings, 1920
Notable cases
[edit]- A 'dwarf' of Punt (ancient Somalia) was given by the Chief clans as partial tribute to the last ruler of Ancient Egypt's Old Kingdom, Pepi II Neferkare (6th Dynasty, circa 2125–2080 BC); it could be inferred that this person was also microcephalic. In a letter preserved at the British Museum, the young king gives instructions by letter, "Harkhuf! The men in your service [escorts; soldiers; sailors; guards, etc.] ought pay sincere care with the dwarf's head while sleeping during the voyage to the palace" (so that it does not fall off). At the same time, it could be for other reasons unrelated to microcephaly, etc.[74]
- Triboulet, a jester of duke René of Anjou (not to be confused with the slightly later Triboulet at the French court).
- Jenny Lee Snow and Elvira Snow, whose stage names were Pip and Flip, respectively, were sisters with microcephaly who acted in the 1932 film Freaks.
- Schlitze "Schlitzie" Surtees, possibly born Simon Metz, was a widely known sideshow performer and actor, who also appeared in Freaks.
- Lester "Beetlejuice" Green, a member of radio host Howard Stern's Wack Pack.
See also
[edit]- Anencephaly (Usually rapidly fatal)
- Cerebral rubicon
- Hydrocephaly
- Macrocephaly
- Seckel syndrome
- Achalasia microcephaly
- Oropouche orthobunyavirus
References
[edit]- ^ "Microcephaly". Health Library: Diseases & Conditions. Cleveland Clinic. April 2023.
- ^ "Microcephaly - Definition of Microcephaly by Merriam-Webster". Archived from the original on 2014-09-14.
- ^ a b c d e f g h i j "NINDS Microcephaly Information Page". NINDS. June 30, 2015. Archived from the original on 2016-03-11. Retrieved 11 March 2016.
- ^ a b "Facts about Microcephaly | Birth Defects | National Center on Birth Defects and Developmental Disabilities". Centers for Disease Control and Prevention. 2016-12-07. Retrieved 2019-07-30.
- ^ a b Faheem, Muhammad; Naseer, Muhammad Imran; Rasool, Mahmood; Chaudhary, Adeel G; Kumosani, Taha A; Ilyas, Asad Muhammad; Pushparaj, Peter Natesan; Ahmed, Farid; Algahtani, Hussain A; Al-Qahtani, Mohammad H; Saleh Jamal, Hasan (2015). "Molecular genetics of human primary microcephaly: an overview". BMC Medical Genomics. 8 (Suppl 1): S4. doi:10.1186/1755-8794-8-S1-S4. PMC 4315316. PMID 25951892.
- ^ Leviton, A.; Holmes, L.B.; Allred, E.N.; Vargas, J. (2002). "Methodologic issues in epidemiologic studies of congenital microcephaly". Early Hum Dev. 69 (1): 91–105. doi:10.1016/S0378-3782(02)00065-8. PMID 12324187.
- ^ Opitz, J. M.; Holt, M. C. (1990). "Microcephaly: general considerations and aids to nosology". Journal of Craniofacial Genetics and Developmental Biology. 10 (2): 75–204. PMID 2211965.
- ^ Behrman, R.E.; Kligman, R. M.; Jensen, H.B. (2000). Nelson's Textbook of Pediatrics (16th ed.). Philadelphia: WB Saunders. ISBN 978-0-7216-7767-5. OCLC 44552900.
- ^ Stoler-Poria, S.; Lev, D.; Schweiger, A.; Lerman-Sagie, T.; Malinger, G. (2010-01-12). "Developmental outcome of isolated fetal microcephaly". Ultrasound in Obstetrics and Gynecology. 36 (2). Wiley: 154–8. doi:10.1002/uog.7556. ISSN 0960-7692. PMID 20069548. S2CID 30379486.
- ^ a b c d "Microcephaly". Stanford Children's Health. Retrieved 2 August 2019.
- ^ "Cephalic Disorders Fact Sheet". National Institute of Neurological Disorders and Stroke. Archived from the original on 2019-07-27. Retrieved 2019-08-02.
- ^ "Microcephaly with Spastic Quadriplegia disease: Malacards - Research Articles, Drugs, Genes, Clinical Trials". www.malacards.org. Retrieved 2019-08-02.
- ^ Ashwal, S.; Michelson, D.; Plawner, L.; Dobyns, W. B. (2009). "Practice Parameter: Evaluation of the child with microcephaly (an evidence-based review)". Neurology. 73 (11): 887–897. doi:10.1212/WNL.0b013e3181b783f7. PMC 2744281. PMID 19752457.
- ^ a b "Microcephaly in Children". Health Encyclopedia. University of Rochester Medical Center. Retrieved 2019-07-30.
- ^ "Microcephaly autosomal dominant". Genetic and Rare Diseases Information Center. Archived from the original on 2020-09-21. Retrieved 2019-07-30.
- ^ Online Mendelian Inheritance in Man (OMIM): Microcephaly 18, Primary, Autosomal Dominant; MCPH18 - 617520
- ^ "Poland syndrome". Genetic and Rare Diseases Information Center. Retrieved 2019-07-30.
- ^ "Microcephaly". World Health Organization. Retrieved 2019-07-30.
- ^ "Trisomy 18: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2020-10-29.
- ^ "Trisomy 13 | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2020-10-29.
- ^ Opladen T, López-Laso E, Cortès-Saladelafont E, Pearson TS, Sivri HS, Yildiz Y, Assmann B, Kurian MA, Leuzzi V, Heales S, Pope S, Porta F, García-Cazorla A, Honzík T, Pons R, Regal L, Goez H, Artuch R, Hoffmann GF, Horvath G, Thöny B, Scholl-Bürgi S, Burlina A, Verbeek MM, Mastrangelo M, Friedman J, Wassenberg T, Jeltsch K, Kulhánek J, Kuseyri Hübschmann O (May 2020). "Consensus guideline for the diagnosis and treatment of tetrahydrobiopterin (BH4) deficiencies". Orphanet Journal of Rare Diseases. 15 (1): 126. doi:10.1186/s13023-020-01379-8. PMC 7251883. PMID 32456656.
- ^ Szczepanski, Sandra; Hussain, MuhammadSajid; Sur, Ilknur; Altmüller, Janine; Thiele, Holger; Abdullah, Uzma; Waseem, SyedaSeema; Moawia, Abubakar; Nürnberg, Gudrun; Noegel, Angelika Anna; Baig, Shahid Mahmood; Nürnberg, Peter (30 November 2015). "A novel homozygous splicing mutation of CASC5 causes primary microcephaly in a large Pakistani family". Human Genetics. 135 (2): 157–170. doi:10.1007/s00439-015-1619-5. PMID 26621532. S2CID 2295608.
- ^ a b c d "Microcephaly in infants and children: Etiology and evaluation". UpToDate. Retrieved 2019-08-02.
- ^ a b c d e f g h i j "Microcephaly - Symptoms and causes". Mayo Clinic. Retrieved 2019-07-30.
- ^ Emily E. Petersen; Erin Staples; Dana Meaney-Delman; Marc Fischer; Sascha R. Ellington; William M. Callaghan; Denise J. Jamieson (January 22, 2016). "Interim Guidelines for Pregnant Women During a Zika Virus Outbreak — United States, 2016". Morbidity and Mortality Weekly Report. 65 (2): 30–33. doi:10.15585/mmwr.mm6502e1. PMID 26796813.
- ^ "Congenital Disorders of Glycosylation". NORD (National Organization for Rare Disorders). Retrieved 2019-08-01.
- ^ "Mito Info". Mito Foundation. Retrieved 2019-08-01.
- ^ "Zellweger syndrome". Orphanet. Retrieved 2019-08-01.
- ^ Reference, Genetics Home. "GLUT1 deficiency syndrome". Genetics Home Reference. Retrieved 2019-08-01.
- ^ "Maternal phenylketonuria". Orphanet. Retrieved 2019-08-01.
- ^ Reddy, Nihaal; Calloni, Sonia F.; Vernon, Hilary J.; Boltshauser, Eugen; Huisman, Thierry A. G. M.; Soares, Bruno P. (2018-05-01). "Neuroimaging Findings of Organic Acidemias and Aminoacidopathies". RadioGraphics. 38 (3): 912–931. doi:10.1148/rg.2018170042. ISSN 0271-5333. PMID 29757724.
- ^ Online Mendelian Inheritance in Man (OMIM): Miller-Dieker Lissencephaly Syndrome; MDLS - 247200
- ^ Joyce, Tina; Huecker, Martin R. (2019), "Pediatric Abusive Head Trauma (Shaken Baby Syndrome)", National Center for Biotechnology Information, AU.S. National Library of Medicine, PMID 29763011, retrieved 2019-07-30
- ^ Donald, Kirsten A.; Walker, Kathleen G.; Kilborn, Tracy; Carrara, Henri; Langerak, Nelleke G; Eley, Brian; Wilmshurst, Jo M (2015). "HIV Encephalopathy: pediatric case series description and insights from the clinic coalface". AIDS Research and Therapy. 12 (1): 2. doi:10.1186/s12981-014-0042-7. ISSN 1742-6405. PMC 4297380. PMID 25598835.
- ^ Tibussek, Daniel; Sinclair, Adriane; Yau, Ivanna; Teatero, Sarah; Fittipaldi, Nahuel; Richardson, Susan E.; Mayatepek, Ertan; Jahn, Peter; Askalan, Rand (2015). "Late-Onset Group B Streptococcal Meningitis Has Cerebrovascular Complications". The Journal of Pediatrics. 166 (5): 1187–92.e1. doi:10.1016/j.jpeds.2015.02.014. PMID 25919727.
- ^ Ramos, Regina; Viana, Rafaela; Brainer-Lima, Alessandra; Florêncio, Telma; Carvalho, Maria Durce; van Der Linden, Vanessa; Amorim, Antonio; Rocha, Maria Ângela; Medeiros, Fabíola (2017). "Perinatal Chikungunya Virus-Associated Encephalitis Leading to Postnatal-Onset Microcephaly and Optic Atrophy". The Pediatric Infectious Disease Journal. 37 (1): 94–95. doi:10.1097/INF.0000000000001690. ISSN 0891-3668. PMID 28737626. S2CID 31790738.
- ^ "Galloway-Mowat Syndrome". NORD (National Organization for Rare Disorders). Archived from the original on 2021-03-11. Retrieved 2019-08-02.
- ^ Kurian, Manju A; Jungbluth, Heinz (July 2014). "Genetic disorders of thyroid metabolism and brain development". Developmental Medicine and Child Neurology. 56 (7): 627–634. doi:10.1111/dmcn.12445. ISSN 0012-1622. PMC 4231219. PMID 24665922.
- ^ Reference, Genetics Home. "Fanconi anemia". Genetics Home Reference. Retrieved 2019-08-02.
- ^ Damlich, Jennifer; Qato, Roa; Cruz, Meredith; Colon, Maria; Wilkins, Isabelle (2009-07-01). "Discussion: 'Microcephaly associated with congenital heart defect' by Barbu et al". American Journal of Obstetrics & Gynecology. 201 (1): e7–e12. doi:10.1016/j.ajog.2009.05.042. ISSN 0002-9378. PMID 19576365.
- ^ "Facts about Microcephaly". Centers for Disease Control and Prevention. 2016-12-07. Retrieved 2019-08-02.
- ^ Crespi, B.; Stead, P.; Elliot, M. (January 2010). "Evolution in health and medicine Sackler colloquium: Comparative genomics of autism and schizophrenia". Proceedings of the National Academy of Sciences of the United States of America. 107 (Suppl 1): 1736–41. Bibcode:2010PNAS..107.1736C. doi:10.1073/pnas.0906080106. PMC 2868282. PMID 19955444.
- ^ Stone, Jennifer L.; O'Donovan, Michael C.; Gurling, Hugh; Kirov, George K.; Blackwood, Douglas H. R.; Corvin, Aiden; et al. (September 2008). "Rare chromosomal deletions and duplications increase risk of schizophrenia". Nature. 455 (7210): 237–241. Bibcode:2008Natur.455..237S. doi:10.1038/nature07239. PMC 3912847. PMID 18668038.
- ^ Dumas L, Sikela JM (2009). "DUF1220 domains, cognitive disease, and human brain evolution". Cold Spring Harb. Symp. Quant. Biol. 74: 375–382. doi:10.1101/sqb.2009.74.025. PMC 2902282. PMID 19850849.
- ^ Rimol, Lars M.; Agartz, Ingrid; Djurovic, Srdjan; Brown, Andrew A.; Roddey, J. Cooper; Kahler, Anna K.; et al. (2010). "Sex-dependent association of common variants of microcephaly genes with brain structure". Proceedings of the National Academy of Sciences. 107 (1): 384–8. Bibcode:2010PNAS..107..384R. doi:10.1073/pnas.0908454107. JSTOR 40536283. PMC 2806758. PMID 20080800.
- ^ "Mosquitos kill more people than any other creature, the CDC warns". NPR.org. NPR Morning Edition. 8 July 2024. Retrieved 6 October 2024.
{{cite web}}: CS1 maint: url-status (link) - ^ "Zika virus - Brazil: confirmed Archive Number: 20150519.3370768". Pro-MED-mail. International Society for Infectious Diseases. Archived from the original on 2016-01-30.
- ^ Rasmussen, Sonja A.; Jamieson, Denise J.; Honein, Margaret A.; Petersen, Lyle R. (13 April 2016). "Zika Virus and Birth Defects — Reviewing the Evidence for Causality". New England Journal of Medicine. 374 (20): 1981–7. doi:10.1056/NEJMsr1604338. PMID 27074377. S2CID 20675635.
- ^ "CDC Concludes Zika Causes Microcephaly and Other Birth Defects". CDC. 13 April 2016. Archived from the original on 31 May 2016. Retrieved 1 June 2016.
- ^ "CDC issues interim travel guidance related to Zika virus for 14 Countries and Territories in Central and South America and the Caribbean". Centers for Disease Control and Prevention. 2016-01-15. Archived from the original on 2016-01-18. Retrieved 2016-01-17.
- ^ Beth Mole (2016-01-17). "CDC issues travel advisory for 14 countries with alarming viral outbreaks". Ars Technica. Condé Nast. Archived from the original on 2016-01-18. Retrieved 2016-01-17.
- ^ Mlakar, Jernej; Korva, Misa; Tul, Nataša; Popović, Mara; Poljšak-Prijatelj, Mateja; Mraz, Jerica; Kolenc, Marko; Resman Rus, Katarina; Vesnaver Vipotnik, Tina (2016-03-10). "Zika Virus Associated with Microcephaly". New England Journal of Medicine. 374 (10): 951–8. doi:10.1056/NEJMoa1600651. ISSN 0028-4793. PMID 26862926. S2CID 205099844.
- ^ Cavallin, Mara; Rujano, Maria A.; Bednarek, Nathalie; Medina-Cano, Daniel; Bernabe Gelot, Antoinette; Drunat, Severine; Maillard, Camille; Garfa-Traore, Meriem; Bole, Christine (2017-10-01). "WDR81 mutations cause extreme microcephaly and impair mitotic progression in human fibroblasts and Drosophila neural stem cells". Brain. 140 (10): 2597–2609. doi:10.1093/brain/awx218. ISSN 1460-2156. PMID 28969387.
- ^ Coley, Brian D. (2013). Caffey's Pediatric Diagnostic Imaging E-Book (12th ed.). Elsevier Health Sciences. ISBN 978-1-4557-5360-4. OCLC 847214216.
- ^ Martin, Richard J.; Fanaroff, Avroy A.; Walsh, Michele C. (2014). Fanaroff and Martin's Neonatal-Perinatal Medicine E-Book: Diseases of the Fetus and Infant. Elsevier Health Sciences. ISBN 978-0-323-29537-6. OCLC 909892605.
- ^ "Aftereffects". Archived from the original on 2009-05-25.
- ^ a b c Kalter, Harold (2010). "Pioneering Studies §Atomic Radiation §Microcephaly and Mental Retardation". Teratology in the Twentieth Century Plus Ten. Springer. p. 21. doi:10.1007/978-90-481-8820-8_2. ISBN 978-90-481-8820-8.
- ^ Burrow, Gerard N.; Hamilton, Howard B.; Hrubec, Zdenek (June 1964). "Study of Adolescents Exposed in Utero to the Atomic Bomb, Nagasaki, Japan". Yale Journal of Biology and Medicine. 36 (6): 430–444. PMC 2604646. PMID 14173443.
- ^ Adams, Hieab H. H.; Hibar, Derrek P.; Chouraki, Vincent; Stein, Jason L.; Nyquist, Paul A.; Rentería, Miguel E.; Trompet, Stella; Arias-Vasquez, Alejandro; Seshadri, Sudha (2016). "Novel genetic loci underlying human intracranial volume identified through genome-wide association". Nature Neuroscience. 19 (12): 1569–82. doi:10.1038/nn.4398. PMC 5227112. PMID 27694991.
- ^ Jamuar, SS; Walsh, CA (June 2015). "Genomic variants and variations in malformations of cortical development". Pediatric Clinics of North America. 62 (3): 571–85. doi:10.1016/j.pcl.2015.03.002. PMC 4449454. PMID 26022163.
- ^ Rash, BG; Lim, HD; Breunig, JJ; Vaccarino, FM (26 October 2011). "FGF signaling expands embryonic cortical surface area by regulating Notch-dependent neurogenesis". The Journal of Neuroscience. 31 (43): 15604–17. doi:10.1523/jneurosci.4439-11.2011. PMC 3235689. PMID 22031906.
- ^ Shen, J; Gilmore, EC; Marshall, CA; Haddadin, M; Reynolds, JJ; Eyaid, W; Bodell, A; Barry, B; Gleason, D; Allen, K; Ganesh, VS; Chang, BS; Grix, A; Hill, RS; Topcu, M; Caldecott, KW; Barkovich, AJ; Walsh, CA (March 2010). "Mutations in PNKP cause microcephaly, seizures and defects in DNA repair". Nature Genetics. 42 (3): 245–9. doi:10.1038/ng.526. PMC 2835984. PMID 20118933.
- ^ Alkuraya, FS; Cai, X; Emery, C; Mochida, GH; Al-Dosari, MS; Felie, JM; Hill, RS; Barry, BJ; Partlow, JN; Gascon, GG; Kentab, A; Jan, M; Shaheen, R; Feng, Y; Walsh, CA (13 May 2011). "Human mutations in NDE1 cause extreme microcephaly with lissencephaly [corrected]". American Journal of Human Genetics. 88 (5): 536–47. doi:10.1016/j.ajhg.2011.04.003. PMC 3146728. PMID 21529751.
- ^ Johnson, Matthew B.; Sun, Xingshen; Kodani, Andrew; Borges-Monroy, Rebeca; Girskis, Kelly M.; Ryu, Steven C.; Wang, Peter P.; Patel, Komal; Gonzalez, Dilenny M.; Woo, Yu Mi; Yan, Ziying; Liang, Bo; Smith, Richard S.; Chatterjee, Manavi; Coman, Daniel; Papademetris, Xenophon; Staib, Lawrence H.; Hyder, Fahmeed; Mandeville, Joseph B.; Grant, P. Ellen; Im, Kiho; Kwak, Hojoong; Engelhardt, John F.; Walsh, Christopher A.; Bae, Byoung-Il (2018). "Aspm knockout ferret reveals an evolutionary mechanism governing cerebral cortical size". Nature. 556 (7701): 370–5. Bibcode:2018Natur.556..370J. doi:10.1038/s41586-018-0035-0. PMC 6095461. PMID 29643508.
- ^ Nowakowski, TJ; Pollen, AA; Di Lullo, E; Sandoval-Espinosa, C; Bershteyn, M; Kriegstein, AR (5 May 2016). "Expression Analysis Highlights AXL as a Candidate Zika Virus Entry Receptor in Neural Stem Cells". Cell Stem Cell. 18 (5): 591–6. doi:10.1016/j.stem.2016.03.012. PMC 4860115. PMID 27038591.
- ^ Li, C; Xu, D; Ye, Q; Hong, S; Jiang, Y; Liu, X; Zhang, N; Shi, L; Qin, CF; Xu, Z (7 July 2016). "Zika Virus Disrupts Neural Progenitor Development and Leads to Microcephaly in Mice". Cell Stem Cell. 19 (1): 120–6. doi:10.1016/j.stem.2016.04.017. PMID 27179424.
- ^ O'Driscoll M, Jeggo PA (July 2008). "The role of the DNA damage response pathways in brain development and microcephaly: insight from human disorders". DNA Repair (Amst). 7 (7): 1039–50. doi:10.1016/j.dnarep.2008.03.018. PMID 18458003.
- ^ Ribeiro JH, Altinisik N, Rajan N, Verslegers M, Baatout S, Gopalakrishnan J, Quintens R (2023). "DNA damage and repair: underlying mechanisms leading to microcephaly". Front Cell Dev Biol. 11: 1268565. doi:10.3389/fcell.2023.1268565. PMC 10597653. PMID 37881689.
- ^ de Koning, T. J. (2006). "Treatment with amino acids in serine deficiency disorders". Journal of Inherited Metabolic Disease. 29 (2–3): 347–351. doi:10.1007/s10545-006-0269-0. ISSN 0141-8955. PMID 16763900. S2CID 35908740.
- ^ Stories, Wander (4 February 2015). Colosseum in Rome: a travel guide and tour as with the best local guide. WanderStories. ISBN 978-9-949-51606-3.
- ^ Mateen, F.J.; Boes, C.J. (2010). "'Pinheads': the exhibition of neurologic disorders at 'The Greatest Show on Earth'". Neurology. 75 (22): 2028–32. doi:10.1212/WNL.0b013e3181ff9636. PMID 21115959. S2CID 207118420.
- ^ "Zip the Pinhead: What is it?". The Human Marvels. 16 October 2010. Archived from the original on 14 April 2016.
- ^ "Interview with Bill Griffith". ZippythePinhead.com. Goblin Magazine. 1995. Archived from the original on 31 January 2012. Retrieved 13 February 2013.
- ^ Kozma, Chahira (10 October 2005). "Historical Review - Dwarfs in Ancient Egypt" (PDF). American Journal of Medical Genetics. 140 (4): 303–311. doi:10.1002/ajmg.a.31068. PMID 16380966. S2CID 797288. Archived (PDF) from the original on 17 May 2017. Retrieved 17 February 2018.










